Time: Noun Is identified as continued progress of existence and events in the past, present, and future, the physics of which, is the measurement of the rotation of earth. Time is expressed in many mediums such as intervals, fixed periods e.g, contractual working day is 8:30am-6:30pm, specific times e.g., board meeting commences at approx. 13:00 GMT. Yet time management is an oxymoron, because we know that time is not what we can control because the clock will continue to tick regardless of how much we constantly have in our day.

As simplistic as we have presented time in the introduction to this article, why is it that too many managers feel overwhelmed, pressured, and stressed by time (of lack of it)? How common is it for you to get to the end of your working day, on the commute home, and to be suddenly met with the damning thought of “what did I actually achieve today”? meaning that you had good intentions and ambitions at the start of the day, but by the end of it, were taken on a differing course, unplanned for too.
To explore this little detail and provide some supporting examples of how you can better control your time. Let us start by introducing the concept that you have total control of your time; it is yours to own. Because time management theory reflects a person’s ability to self-manage their time.
What your time meets along its daily journey are obstacles, challenges, and sometimes outright time thief’s, some of which blind side you, as they are unintended consequences of your role. How do you recognise these, overcome them, and better manage your time throughout the day?
We will work with the concept that you have the skills to organise and align your task, and not your time? For time is a constant, but task and their requirements are the variables. When supporting many organisations and their leaders to implement and redesign new ways of working, I am met with the most common phrase I hear “I would love to do that, but I just don’t have the time for it” …first challenge back is that they do have time, they are unsure of how to prioritise it accordingly.
To get to this state though, one must not underestimate how much time they are a victim to the emails, which is the most common source of task delivery in model age – along with its new companion, WhatsApp! We know detail of emails of the likely contenders for disrupting time, too many come in to the inbox, too many are lacking in clarity around what you are meant to do with them, too many are sent on distribution lists, and you are unsure if it was meant for you in the first instance.
How others send emails, you cannot be accountable for, however the volume of time you spend on emails and procrastinating about what to do with it, it within your control. A way to take control is to create categories for your emails – like colour coding them to be able see at quick glance which ones require your attention. This is how you apply the theory of Steven Covey Time Management Matrix where you need to be able to understand the ask.
With your categories, try not to map more than ten of them, as this will help to keep your management of them as they enter your inbox concise, with no email being attributed more than a couple of tags. The example as shown herein:
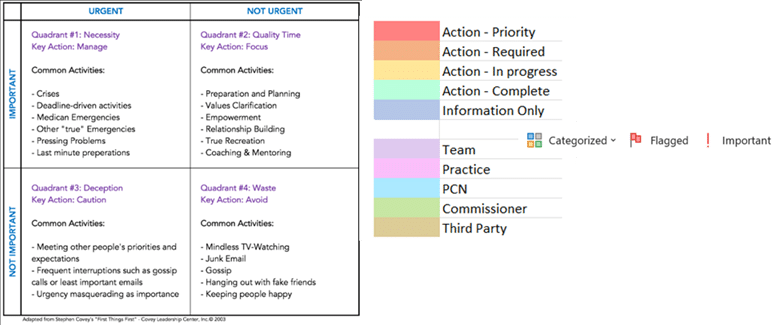
Another time pressing matter, is that of meetings, lots of them, invites for meetings, that someone else decided you should be added to the list, it’s an invite, which means you are not at liberty to attend, unless you have been briefed on the “why you” and what you are to contribute. Too many managers attend meetings because it is in their diary. Accompany sub folders in your emails to the categories approach will help you clear out the action completed and the information only items from your main email list.
TOP TIP: Do not check emails – process them and apply the tag: Action tags, should be then applied “moved” into your diary so you have allocated the time to complete this task.
It is fascinating to observe the desire to be good at time management and how our trusted old “to do lists” are getting in the way of achieving that.
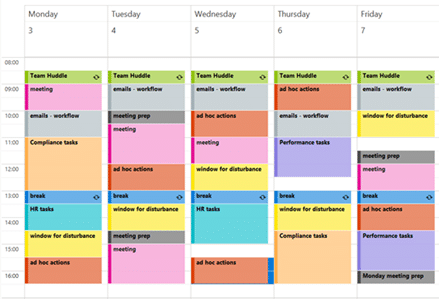
I question when you have a to do list, are you writing next to each item how long it will take, and over what time you must complete it? If the answer is no, then it is time to reset your default way of working and consider a movement of “to do lists” or “task lists” into a diary where time allocation can occur, as per the example shown herein.
Taking this time management approach will help you to shift from fighting fires and buckling under the pressure of perceptions of tasks being urgent, to that of ones which are not urgent but are important, for you to be working through. It will also help you to articulate to others the expectations and the boundaries at which you work within.
TOP TIP: Ditch the “task list,” and “Diarise the do-list,” oh and allow for “wriggle room” in your diary, this gives you breathing space to make
So many meetings, are they a waste of time? To help you better understand whether you should attend as many meetings as you do ask yourself this question: “Does the meeting invite have an agenda?” If the answer is no, do not accept the invite until it does. Why recommend you take this stance? How can you make an informed decision about where best to place your time if you are not cited on the topics and agenda items, to know whether you can contribute and thus give value or indeed take value from attending. Meetings, that run over, that are not being chaired properly, do you stay in them and continue to eat into more of your time, when you were given a meeting time and feel bad for leaving early, when you are leaving at the time the chair was meant to close the meeting.
According to research the average meeting lasts for two hours, and many have at least one meeting a day in their diary, which means for a whole-time member of staff they spend 26.66% of their working week, in meetings, challenge yourself on whether this is you and whether they are worth giving up over a quarter of your weekly time for.
TOP TIP: A way to help you understand whether you should be attending meetings or not, is to do the maths quite simply on the cost of your attendance, and that of colleagues in local meetings, and to ask the question if the cost was worth its return on investment?
Pay attention your minds attention management. Attention to detail is finite, humans can only concentrate at the top of our game for brief period “power hour” I usually refer to them as. By design anything that you continue to work on for too long, will cause your memory to lapse, or cause you to work in a heuristic manner, which can alter information processing and memory.
Recognise this within yourself, reflect on the types of tasks you are achieving when you are in a state of proactive attention, which is where you are fully focused, alert and in the zone, acknowledge at what times of your working day? What tasks are you trying to work through when you have an active attention, the times of the day when you are ticking along but perhaps attention has been stretched slightly and you are lagging slightly, where focus dips in and out, and you are quite content to be distracted.
Finally recognise when you have reached an inactive attention state, where the tank is running on empty, lacking in functional brain power to complete cognitive tasks, clear decision making, likely your input at this stage is not too valuable…
Is this the time to switch off the lights and go home. If you work beyond your working hours regularly, you are a suitable case study to be implementing some, if not all these recommendations herein.
TOP TIP: Time to leave you with some quotes to reflect on:
• Time is precious – true
• Time is money – false
• Time waits for no one – true
• Time flies – false
Author: Joanna Fox l Associate Consultant l Primary Care Commissioning.
Primary Care Business, Human Resources, and Human Factors Specialist
Last Updated on 1 February 2023
